Understanding the G614 Variant's Impact on Covid-19 Fatalities
Written on
Chapter 1: The Evolution of SARS-CoV-2
SARS-CoV-2, the virus responsible for Covid-19, evolves similarly to other viruses. An early bioinformatics analysis identified mutations in SARS-CoV-2 strains isolated in Italy. Another phylogenetic study, which I previously discussed, highlighted three distinct clusters of the virus, with isolates from Italy and Iran forming a unique group compared to other regions.
As research progressed, scientists began to categorize the various SARS-CoV-2 variants. It’s important to note that not all variants carry significant medical implications; some mutations do not affect the virus's functionality. However, the G614 variant has garnered considerable interest within the scientific community.
This article does not focus on the preprint study suggesting that the G614 mutation increases transmissibility, which has generated debate.
Section 1.1: G614 Variant and Case Fatality Rates (CFRs)
Researchers in the United States conducted a bioinformatics study that reported, “The variant 23403A>G (p.D614G) in the spike protein B-cell epitope is frequently found in European nations such as the Netherlands, Switzerland, and France, but is rarely detected in China.”
The D614G mutation is characterized by a change in the amino acid at position 614, shifting from aspartic acid (D) to glycine (G), hence the designation D-614-G. This mutation leads to two variants: D614 and G614, indicating the presence of either D or G at position 614.
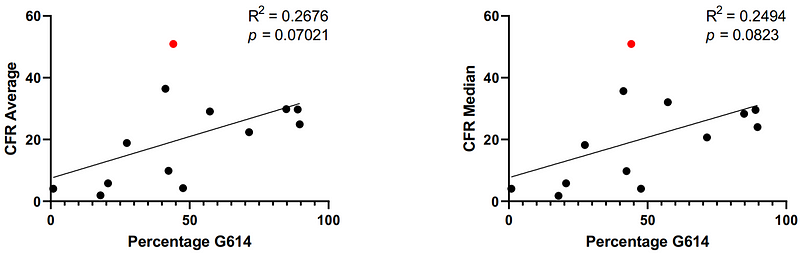
A subsequent study published in May built upon these findings, linking the prevalence of the G614 variant to Covid-19 case fatality rates (CFRs) across twelve countries. European nations like Italy, Belgium, and France exhibited the highest prevalence of the G614 variant, while countries in the Far East, including China, Australia, and Japan, had the lowest prevalence.
The correlation between G614 variant prevalence and CFRs was notably strong. For instance, the study noted that less than 1% of recorded viruses in China were the G614 variant, coinciding with the country's second-lowest average CFRs.
The data further elucidates the higher mortality rate in New York compared to other U.S. states. The prevalence of the G614 variant in New York was found to be 82.5%, with total deaths reaching 6,268 as of April 9, 2020. In contrast, states like Washington, Oregon, and California reported significantly lower G614 prevalence (16.3%, 25%, and 26.7%, respectively) and death tolls (431, 38, and 507, respectively), indicating a stark difference in fatalities within Western U.S. states.
The authors acknowledged limitations in their analysis, noting that factors such as disease comorbidities, diagnostic testing practices, and social distancing measures may vary across countries. Additionally, the United Kingdom exhibited unusually high CFRs, which weakened the correlation strength from a statistically significant R² of >0.45 to a non-significant R² of >0.2.
Free-access source: Becerra-Flores M, Cardozo T. SARS-CoV-2 viral spike G614 mutation exhibits higher case fatality rate [published online ahead of print, 2020 May 6]. Int J Clin Pract. 2020;10.1111/ijcp.13525. doi: 10.1111/ijcp.13525
Section 1.2: G614 Variant and Molecular Modeling
The same Langone Health study conducted biophysical molecular modeling of SARS-CoV-2 variants. It found that compared to the original D614 variant, the G614 variant exhibits a less stable spike protein. Consequently, the G614 variant has a lower binding affinity to host cell receptors and is considered less infectious, although the extent of its transmission capacity remains undetermined.
The authors suggested that the G614 variant's increased fatality rate may be attributed to immunological factors rather than virological ones. They wrote, “The form that binds the receptor less effectively is also better shielded from the host immune system.” This implies that the immune response may generate ineffective antibodies against the G614 variant, allowing it to evade detection more successfully than the D614 variant. Notably, this evasion strategy is not unique to SARS-CoV-2; similar tactics are employed by viruses like HIV and respiratory syncytial virus (RSV) to evade immune responses.
Chapter 2: Implications for Vaccine Development
Whether the G614 variant will be classified as a new strain of SARS-CoV-2 is still a matter of debate. Any genetic change in the virus can be categorized as a variant, but to qualify as a strain, it must demonstrate a distinct biological function.
If the G614 variant meets this criterion, it could complicate vaccine development. Richard A. Stein, a professor of medicine and director of the Urban Community Cardiology Program at New York University, expressed concerns in an editorial response to the Langone Health study. He noted, “The immediate questions revolve around how these mutations affect vaccine efficacy and whether there is a need to create multiple candidate vaccines that address a variety of epitopes and their variants.”
Returning to the U.S. study identifying the G614 variant, the authors warned that “the highly prevalent G614 variant in the European population may lead to antigenic drift, resulting in vaccine mismatches that provide limited protection to that demographic.” Such considerations are critical in designing a universal vaccine aimed at combating one of the deadliest outbreaks of the century.
For further insights into the implications of the G614 variant on the Covid-19 pandemic, please refer to:
- What the D614G Mutation Means for Covid-19 Spread, Fatality, Treatment, and Vaccine
- Real-life implications of the global transition from the D614 to G614 variant.